The best investment you can make to get the success you expect, one medical record at a time.
This is a fictitious situation and report developed for the sole purpose of demonstrating examples of report format and length. For confidentiality reasons, this report bears no resemblance to any actual case. Actual reports will vary in format and length appropriate to ease type and complexity as determined by legal nurse consultant and attorney-client.
May 6, 0000
Top Attorney
Attorney at Law
RE: Ms. Amy Client, injured
Dear Mr. Attorney:
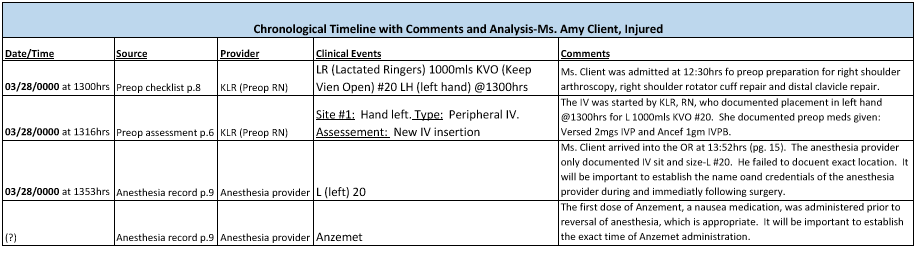
Pursuant to your request, I have screened the hospital medical records of Ms. Client for the period 3/26/0000-4/05/0000, including records from preop holding, OR, PACU (Post Anesthesia Care Unit), ASU (Ambulatory Surgery Unit) and ED. I have included my comments and recommendations for your consideration.
Ms. Client is a 33-year-old white female who was admitted 3/28/0000 at 1312 for uneventful right shoulder arthroscopy. During recovery she sustained a complication of IV therapy.
In my opinion, this case is meritorious because there was failure to timely diagnose and treat phlebitis, thrombophlebitis and extravasation following administration of IV Anzemet. These deviations resulted in compartment syndrome and permanent injury to Ms. Client's nerves and muscles in the left forearm. She currently has pain, numbness and inability to grasp objects.
I noted numerous discrepancies in the documentation of the IV site. Ms. Client's IV was started in the left hand in the preop area at 1300 and remained in the left hand throughout the surgery. The PACU nurse documented at 1525 that the IV was in the left forearm.
However, there is no documentation of site change anywhere in the medical record. When Ms. Client was transferred to the ASU at 1625, the ASU nurse documented that the IV was in the left hand. It will be important to establish whether the IV was in the left hand, left forearm or both while Ms. Client was in the OR, PACU and ASU. This sloppy documentation is a significant deviation from the standard of care and makes it difficult to analyze this incident in its entirety.
Ms. Client was transferred from the OR to PACU at 1525. The PACU nurse administered Anzemet (which is given to control nausea) at 1611. According to Ms. Client, she complained of excruciating pain and burning following administration of Anzemet. Anzemet IV was also administered in the OR (exact time not documented) and there is no documentation of any issues with this Anzemet administration.
The PACU nurse failed to document Ms. Client's complaints and failed to assess and recognize complications of IV medication administration. She failed to report Ms. Client's complaints to the doctor.
Ms. Client was transferred to the ASU at 1625. The PACU nurse failed to report the status of the IV site to the ASU nurse. The ASU nurse documented that the IV was in the left hand, which conflicts with the PACU nurse, but is consistent with the OR nurse.
The ASU nurse documented at 1630 that Ms. Client had hives on her left hand and forearm. This initial assessment by the ASU nurse strongly suggests that the hives were present in the PACU, even though they were not documented by the PACU nurse. The ASU nurse notified the doctor and administered 25 mg Benadryl at 1635 in the left hand. This nurse should have administered Benadryl at a different site. She documented at 1730 that Ms. Client denied itching and that hives were subsiding on the right (late entry: corrected to "left") forearm.
The ASU nurse documented that the IV was discontinued at 1740 and that there was no evidence of redness or swelling at the IV site. In view of Ms. Client's return to the ED on 3/29/0000, it is unlikely that there was no redness and swelling at this time. Ms. Client was discharged home at 1755 with instructions to call the doctor if she had severe pain, numbness of hand, temp. 101 or above. I recommend evaluating this entry for possible tampering. Additionally the ASU nurse failed to instruct Ms. Client how to care for her left hand and forearm. The ASU nurse should not have discharged Ms. Client in her condition.
Ms. Client returned to the ED on 3/29/2012 at 0840 with "edematous left hand with ecchymosis and coolness since yesterday."
She was taken to the OR where she underwent fasciotomy of the hand with carpal tunnel release and fasciotomy of the foreann. She returned to the OR on 3/31/0000 4/2/0000 and 4/4/0000 for irrigation and debridement of the left hand and forearm. She was discharged on 4/5/0000. There is no evidence of significant deviations from the standard of care during this second hospitalization.
The defense will probably argue that the incident was unavoidable and was due to a rare, unexpected adverse drug reaction. Even if they are successful with this position, the healthcare providers failed to respond timely and appropriately to the adverse drug reaction. Their significant deviations resulted in permanent injuries.
I recommend expert review of this case by a PACU nurse, an anesthesiologist and a vascular surgeon. I also recommend a more detailed, moderate report that would include a detailed chronological timeline to assist you in developing this case. Interviewing Ms. Client would be extremely valuable in my further development of this case.
In conclusion, thank you for the opportunity to consult on this case. I will follow up within two days to answer any questions about the case and determine the next steps you would like me to take. Very truly yours,
Michele Webber RN, CLNC
Chronological Timeline of events shown below: